What is brachytherapy?
Brachytherapy is a non-surgical method of treating cancer where we place tiny radiation sources directly into the prostate and tumour in order to kill the cancer cells.
The name comes from the Greek word for short distance and refers to the way that the radiation is contained so that it can only affect tissues in the immediate vicinity – hence, a short distance. This is opposed to other forms of radiotherapy that are more indiscriminate and can cause collateral damage to healthy tissue.
How it works
It has long been known that radiation can kill cancerous tumors. The problem has always been the effect the radiation can have on other healthy tissue.
Brachytherapy seeks to avoid damage to healthy tissue by delivering the radiation directly to the site of the cancer.
There are two ways we can achieve this, both fairly similar.
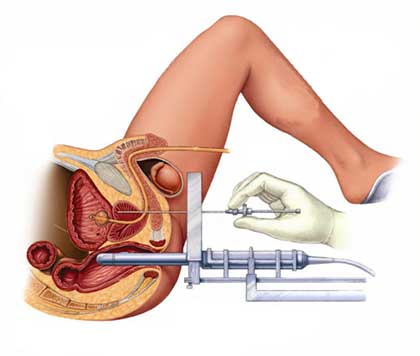
Both involve the placement of hollow needles directly into the prostate. This is done under general anaesthetic. An ultrasound probe is placed in the rectum to guide the urologist or radiation oncologist performing the implant procedure. Then needles are guided into the prostate between the base of the scrotum and the anus – an area called the perineum.
Prostate Seed Implant (Low dose rate brachytherapy)
Brachytherapy techniques allow delivery of much higher radiation doses into the prostate than can be achieved by standard external beam radiation techniques. This gives the potential for improved long term local cancer control. At the same time there is less dose received by the rectum, which can potentially decrease the risk of long-term rectal complications.
Brachytherapy techniques also allow dose escalation delivery of higher doses of radiation directly into the known tumour areas of the prostate.
The lack of randomised trials between brachytherapy and surgery makes it difficult to compare these modalities with respect any difference in long term cancer specific survival. Nevertheless, the published data on brachytherapy shows a similar 15 year overall and cancer specific survival rates to a radical prostatectomy. There does appear to be less risk of early impotence and incontinence of urine with brachytherapy, although these differences become less pronounced 10 years after treatment. There is a higher risk of bladder filling symptoms and burning in the urine (dysuria) following a brachytherapy implant compared with a radical prostatectomy. Brachytherapy obtained a Medicare rebate in Australia 2003 which increased its popularity; however the numbers brachytherapy procedures have decreased over the last decade consistent with the increased uptake of surgery with robotic radical prostatectomy technology or external beam radiotherapy using modern image guided techniques.

External Beam radiotherapy (IMRT)
External beam radiotherapy in Australia has traditionally been the main treatment option for locally advanced prostate cancer, or in patients with localised prostate cancer that are considered as not suitable (medically unfit) to undergo a radical prostatectomy. The improvement in delivery of radiotherapy with image guided techniques has allowed for an increase in the dose delivered to the prostate, without significantly increasing the risk of damage to surrounding structures, such as the bladder and rectum. Based on overseas data, this radiation dose escalation (particularly with doses of 78Gy) has resulted in improved long term local control and decreased PSA failure compared with standard radiotherapy techniques used over 15-20 years ago. IMRT cannot deliver doses to the prostate as high as with a brachytherapy implant / boost.
The complications of IMRT include chronic rectal symptoms, such as frequency / urgency of bowel motions, rectal mucus production and bleeding form the rectum / urine.
High Dose Rate Brachytherapy
Increasing the radiation dose delivered to the prostate (radiation dose intensification) has led to improved long term local control and biochemical freedom from recurrence of prostate cancer. One method of radiation dose intensification is with high dose rate prostatic brachytherapy, via the use of iridium 192 source, delivered via temporary transperineal HDR brachytherapy needles inserted into the prostate.
In Australia high dose rate brachytherapy is usually performed with three fractions of radiotherapy, (usually 7Gy per fraction), delivered to the prostate over a 30-hour period via the brachytherapy rods inserted into the prostate via the perineum. The perineum is the area between the scrotal sac and the rectum. More recently some centres have changed to a single fraction of 15Gy. Thereafter external beam radiotherapy is delivered to the prostate on a daily basis over a 5week period (46Gy in total) . This increases the intra-prostatic prostate radiation dose compared with standard radiotherapy IMRT techniques.
Each State in Australia has a centre with the ability to perform high dose rate brachytherapy.
Our unit at the Wesley Hospital in Brisbane has performed > 1200 HDR brachytherapy procedures since our first procedure in August 2000.
HDR brachytherapy is performed for high-risk prostate cancer, or patients with multiple intermediate risk factures, who are assessed as not appropriate for a radical prostatectomy procedure.
The potential complications of HDR brachytherapy include, but are not limited to, a 5 – 10% risk of a urethral stricture and a >50% risk of impotence.
Benefits of brachytherapy over other treatments
- Because brachytherapy is so localised, we are able to use higher doses of radioactivity than with traditional radiotherapy. This leads to a faster result with fewer ill effects on surrounding tissues.
- A brachytherapy session usually takes no more than 2 hours and often less.
- Patients can return to work within a day or two of the procedure.
- Brachytherapy is non-invasive and has been shown to have less side effects on urinary and sexual function.
Am I a brachytherapy candidate?
Brachytherapy is only appropriate in a certain set of circumstances.
In general, my criteria for a low dose rate brachytherapy candidate are:
- Low risk cancer
- Gleason score under 6
- PSA under 10
- Little or no urinary symptoms
- Likely to live more than 10 years
- Prostate smaller than 50 grams
- Age above 60 years
In general candidates for high dose rate brachytherapy are men with large volume high grade cancers, i.e. Gleason score 8-10, a PSA level of >10 and a palpable nodule in the prostate on rectal examination that appears to extend beyond the wall of the prostate. This group of patients are sometimes considered not suitable for surgery, especially in the older age group.
Each case is, however, taken on its merits.
Would you like to discuss brachytherapy?
Make an appointment so we can discuss this treatment and see if it is right for you.
